Bridging the Divide: Right Treatment, Right Patient, Right Time
As clinicians, we often find ourselves navigating a landscape in pain medicine that is as ideologically charged as any political debate. My own recent experience—reading an article sharply critical of spinal cord stimulation—reinforced for me how quickly pain management discourse can become polarized, with interventions being cast as inherently good or bad, much as we see in the wider world’s political arenas. It’s tempting to gravitate towards certainty, to stake a claim on one “side” of treatment philosophy and plant our flag. But the reality we inhabit with patients is far more nuanced, requiring a shift from rigid dogma to thoughtful matching.
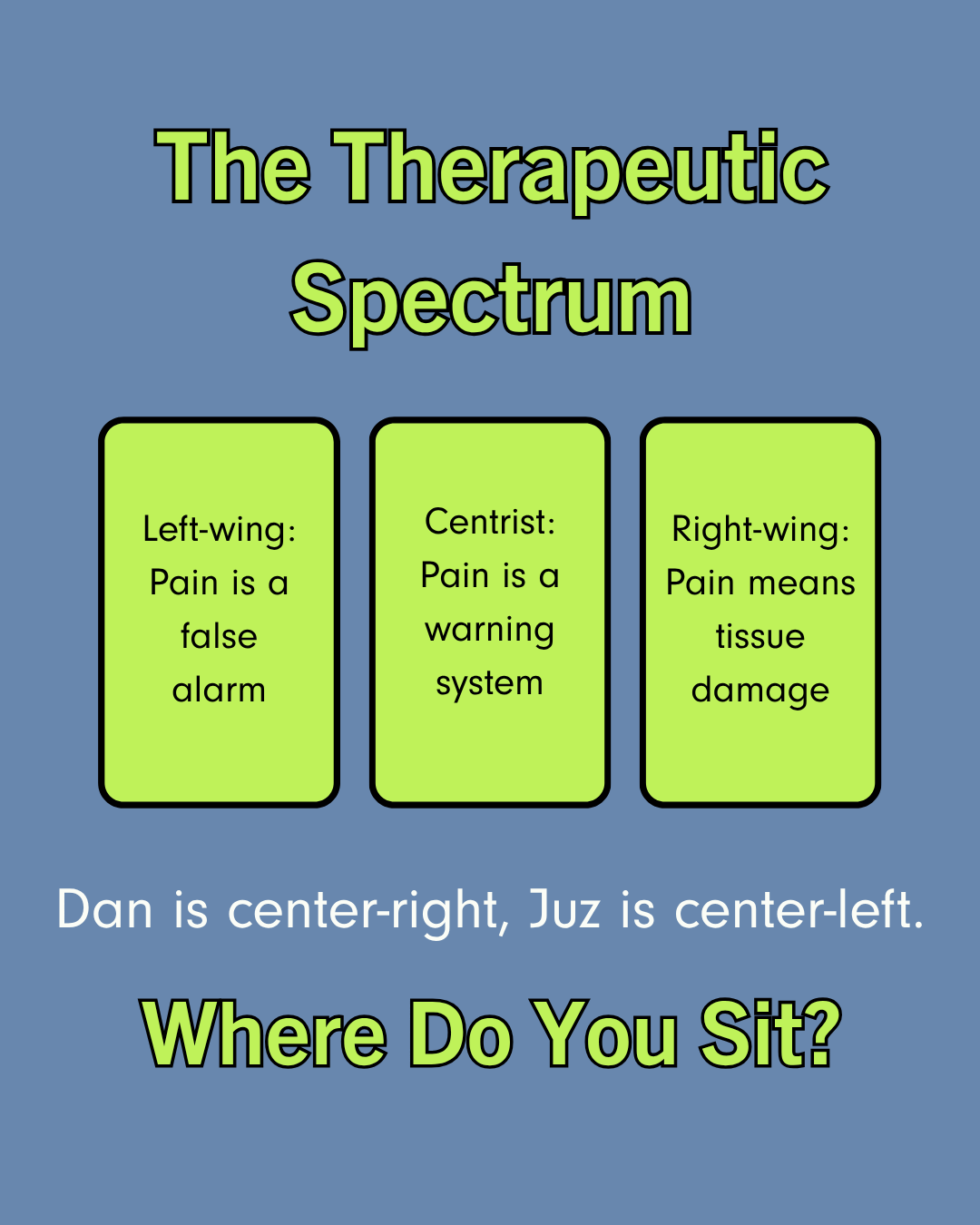
Pain like Politics
In reflecting on these debates, I find that the language and postures used echo political spectrums. Some approaches in pain medicine, for example, tend toward the “pull yourself up by your bootstraps” mentality—pain as a personal failing that should be met with individual fortitude and self-correction. Others adopt a more communal, system-based lens: pain is seen as an outcome of external factors and thus addressed through systemic interventions and collective responsibility. And of course, there are those who stand somewhere in the pragmatic middle, looking for elements of value in both perspectives.
The Therapeutic Spectrum
But just as with political ideologies, no single treatment philosophy is a one-size-fits-all solution. The question should not be, “Which camp is right?” but rather, “Which approach is right for which patient?” Our patients are not categories; they are individuals with expectations, experiences, and psychological frameworks that make certain philosophies of care more effective for them than others. Context matters. A patient searching for agency may resonate more with self-management techniques, while another overwhelmed by structural barriers with more focal, physical drivers may need systemic support before individual strategies can succeed.
This is where humility and flexibility become our allies. Rather than rushing to defend or attack a particular intervention or school of thought, we do better by asking—out loud and with our patients—what narrative fits their worldview and what approach might be workable for them now.
Our Takeaway For You
Our role is less about being missionaries for a cause and more about being matchmakers, pairing patients’ needs and values with the most constructive element from a diverse treatment toolkit.
In this light, pain medicine becomes less a battlefield of right and wrong, and more a marketplace of options where the best outcome is determined through thoughtful alignment, careful listening, and respect for complexity. We serve our patients best by moving beyond rigid positions and instead honing our craft of clinical matchmaking, understanding that success is defined not by the purity of our ideology, but by the fit between treatment and the person seeking relief.
Let us not mimic the divisiveness that so easily infects public discourse. Instead, let’s remain steadfast in our commitment to nuance and patient-centered care, recognizing that the right treatment is not a universal absolute, but a personal match.
For more insight and practical advice, listen to episode 33 of It’s Not in Your Head Podcast, or watch on YouTube.